Patients coping with the stresses of cancer can experience depressive symptoms, with an estimated 22% to 29% of newly diagnosed patients experiencing major depressive disorder (MDD; Raison CL, Miller AH. Biol Psychiatry. 2003;54:283-294). To help these patients, a group of psychologists devised a combined biobehavioral intervention (BBI)/cognitive behavior therapy (CBT).
Reporting in the Journal of Consulting and Clinical Psychology, Brittany M. Brothers, PhD, and colleagues at The Ohio State University demonstrated a significant decline in depressive symptoms among patients with MDD undergoing BBI/CBT. Beginning with an intervention previously designed by the team, Brothers and colleagues offered sessions to patients with a current or previous cancer diagnosis who also had MDD as a primary diagnosis.
Patients underwent 12 weekly individual sessions, with those not attaining remission continuing for another 4 weeks of BBI/CBT. If remission remained unachieved, 4 more weekly sessions were offered, for a total of 20. “The good news is that the treatment worked just as well for [those patients with more severe depressive symptoms],” Brothers tells the Academy of Oncology Nurse Navigators. “They just needed more treatment—additional sessions—to achieve remission.”
The results are impressive. Analyses using data from all patients showed a significant decline over time in depressive symptoms. Of 21 patients completing the intervention, 19 achieved remission of their MDD. These improvements in mental health functioning appear to be independent of physical health, with half of patients experiencing disease progression or a major medical event during the intervention period.
And the team’s use of rigorous scientific methods strengthens their results. Psychiatric diagnostic status was assessed using the Structured Clinical Interview for DSM-IV (SCID), and depressive symptoms using the 17- item Hamilton Rating Scale for Depression. In addition, patients self-reported their depression using the Beck Depression Inventory—Second Edition, and therapists assessed cancer-related traumatic stress using the Impact of Events Scale, history of past depressive episodes using the SCID, health-related quality of life using the Medical Outcomes Study Short Form-36, the patient’s pain and its interference in functioning using the Brief Pain Questionnaire, and fatigue and its interference with functioning using the Total Disruption Index of the Fatigue Symptom Inventory.
The Intervention
Since 1994, Barbara L. Andersen, PhD, has studied the impact of cancer-specific stress on comorbidity and mortality. Using that biobehavorial model of cancer stress, the team, led by Andersen, developed the combined BBI/ CBT intervention. For the current study, they designed a manual through which postdoctoral fellows and predoctoral clinical psychology graduate students provided therapy tailored to patient characteristics.
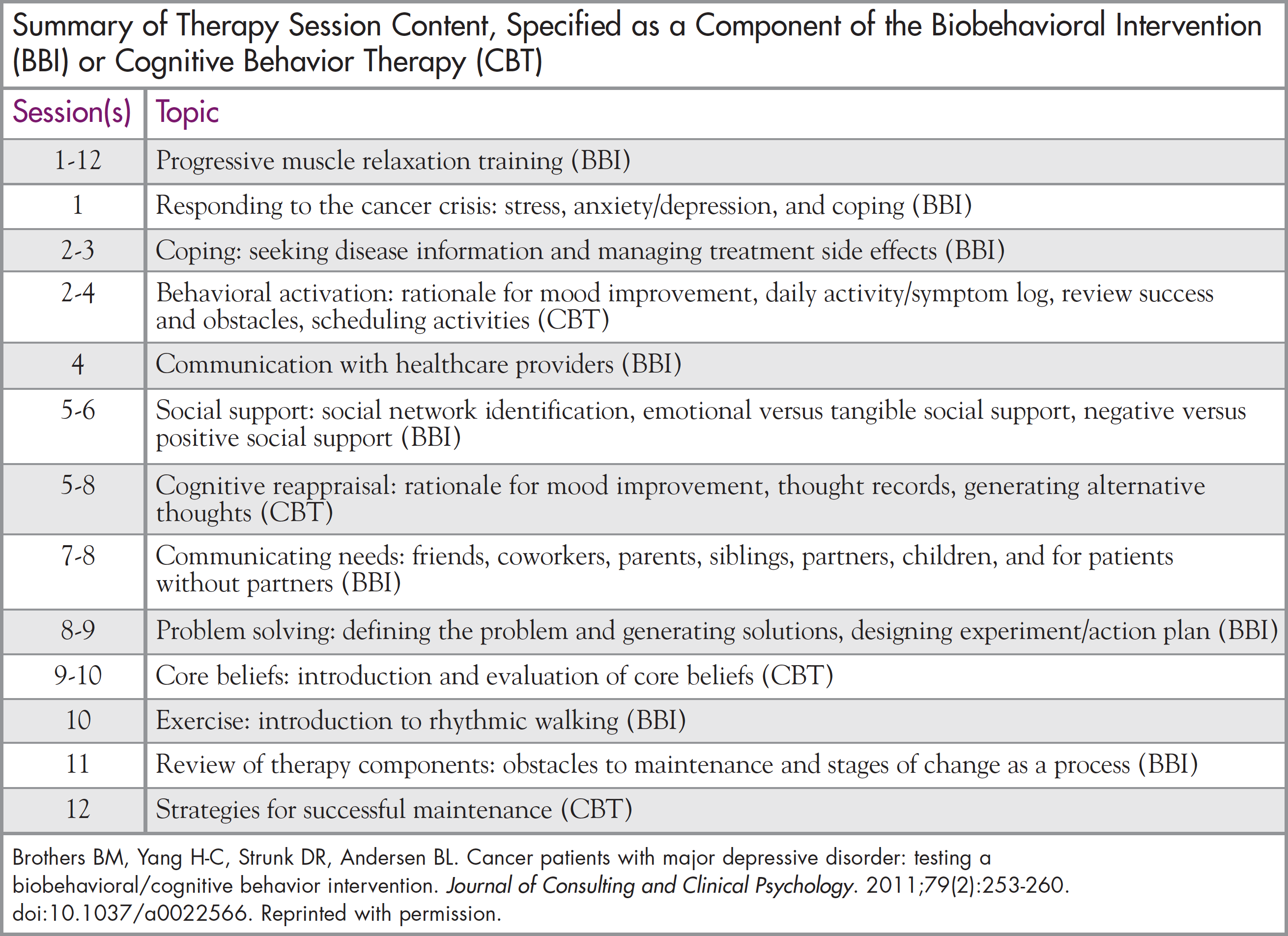
Coping strategies to improve the mental health and health-related quality of life of cancer survivors were taught over 12 sessions or longer, as needed. Most strategies offer direct assistance with the interrelationship among psychological, behavioral, and biologic factors relevant to the progression of cancer. Some strategies are borrowed from traditional therapy to address anxiety and depressive emotions. A detailed description of the BBI, which further delineates the 2 methods of therapy and how they can be combined for the cancer population, was published by Andersen previously (Cogn Behav Pract. 2009;16:253-265).
Implementing the intervention was not without challenges. One major complication was cancer treatment itself. For some patients, undergoing chemotherapy created “too much stress to start the psychological intervention [during therapy],” says Brothers. For others, “it was difficult energy-wise to travel to multiple clinics, because our clinic was not located at or near the oncology clinic.” Out of the 36 total patients enrolled, 15 failed to complete therapy. On average, noncompleters attended 11 sessions. The study suggests that patients most at risk of dropping out include younger patients, those with a gynecologic cancer, those currently undergoing chemotherapy, and those experiencing recurrence.
Nursing Implications
Although this intervention should be led by mental health professionals, nurses and other navigators have a pivotal role in assisting their patients with MDD, says Brothers. “They can encourage patients who are on the high end of the stress scale to learn these effective coping skills. Having nurses and navigators educate patients that [the coping skills taught with BBI/CBT] are beneficial treatments, in the long term, can help with their medical treatment.”
Nurses, in particular, are essential in identifying those patients who are at risk for depression. Although she has not performed any research on the topic, Brothers suggests that the literature supports such risk factors as a lack of a spouse or partner, lower levels of social support, hopeless feelings, young age at diagnosis, as well as patients who are of lower socioeconomic status or part of an underserved population. In addition, patients with a concurrent anxiety disorder are at very high risk, as well as those with previous episodes of depression. Brothers gave this example to help nurses identify these patients: “This would be individuals who have intrusive thoughts, such as thoughts that pop into his or her mind even when a cancer patient was trying not to have them, or having recurrent dreams and images.”
Navigators, for their part, can help by working with local mental health professionals to make access to the intervention easier. Brothers gives this illustration: Navigators can help coordinate care to minimize patient travel time and burden. For instance, they can arrange for appointments to be offered at a convenient location, such as having the community mental health practitioner use an office in the oncology suite or next to the chemotherapy unit, so patients can receive both services, one after the other.
Future Research and Training
Now that the preliminary study is complete, the team is working on 2 goals. “We are working on a grant to perform a randomized study, and we have a grant submitted to develop a training institute,” says Brothers. The team has received numerous requests from mental health practitioners who want to learn about the intervention for cancer-related stress and how it is adapted for patients with depression. Hopefully, in the future, all patients with cancer and MDD will benefit from this research. “We would be very excited to offer that training,” concludes Brothers.




