In preparation for the new American College of Surgeons Commission on Cancer (CoC) standards,1 OSF Saint Anthony Medical Center focused on having an oncology nurse navigation program in place to support patients by January 2014. The Center for Cancer Care at OSF Saint Anthony Medical Center is a comprehensive cancer center located in an urban setting in the Midwestern United States. The most recent CoC site survey was conducted in September 2011, and the center received accreditation with commendation. The center also received the CoC Outstanding Achievement Award for the 2011 survey. The current volume of patients is approximately 850 analytical new cases per year.
The new CoC standards require that a patient navigation process be in place by 2015. The standards concentrate on individualized assistance for patients with cancer to overcome common barriers encountered in the healthcare system. The standards aim to ensure that patients have access to psychosocial support through distress screening and appropriate referrals. In addition, the standards define requirements for survivorship care planning for patients completing cancer treatments.
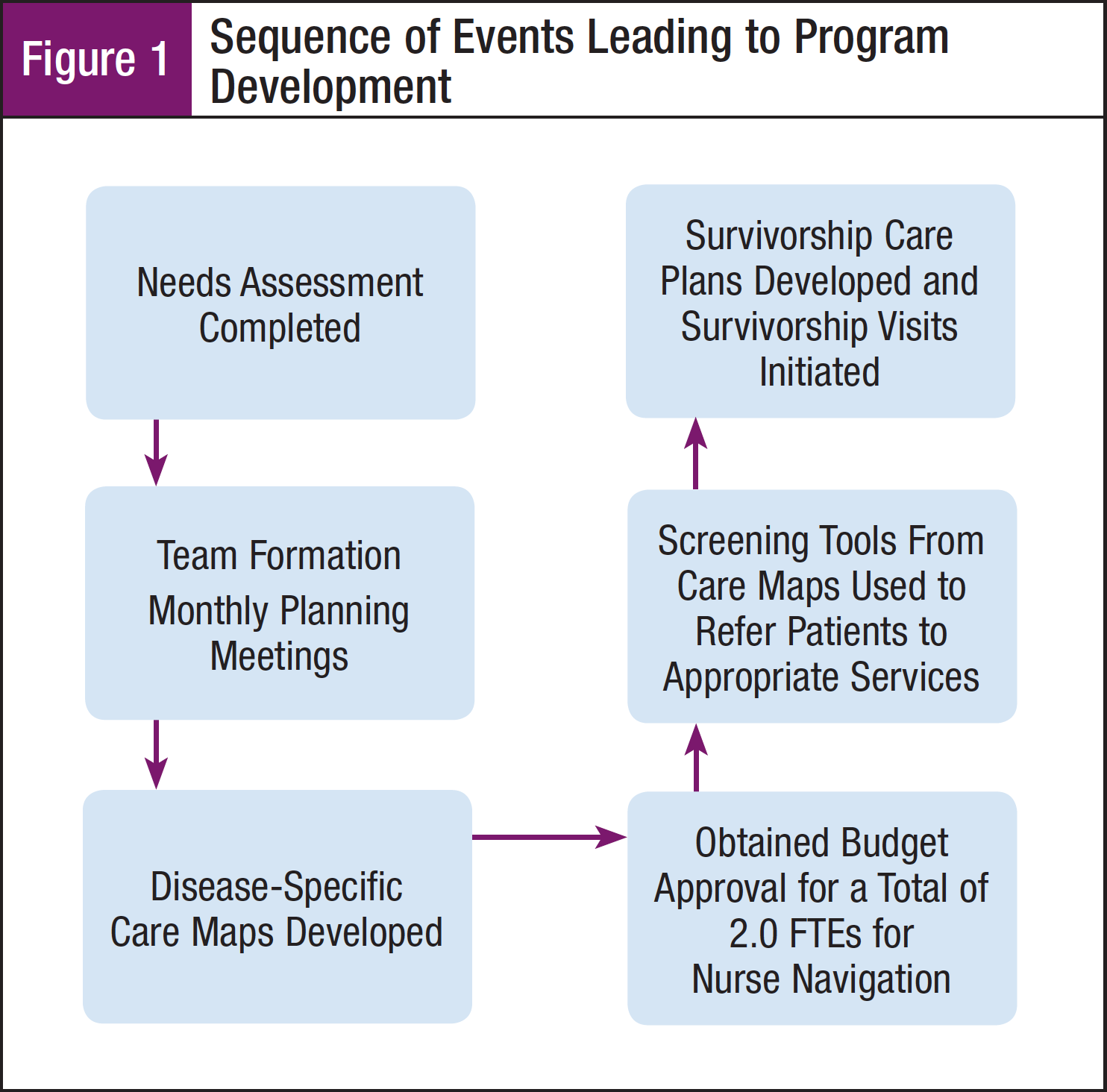
Extremely positive anecdotal feedback from a 4-year pilot program using an oncology nurse navigator (ONN) for breast cancer patients prompted the center to pursue the development of an oncology nurse navigation program. In order to build a stronger program, actions were taken to restructure the framework of the program to meet specific patient care needs, to comply with the new CoC standards, and to positively affect outcomes. The center developed a collaborative action plan using a step-by-step framework (Figure 1).
This article will focus on the steps taken to launch and develop an oncology nurse navigation program.
Getting Started: Creation of a Small Work Group
The concept of oncology nurse navigation in cancer care has been recognized as a vital, supportive component of patient care on the care continuum by the oncology community. Patients with cancer perceive ONN services as effective augmentations in the areas of patient education, timely care, community resource referrals, and mobilizing financial assistance.2,3 Key stakeholders, including the department director, medical oncologists, and the ONN currently involved in the pilot program, met in a work group format on a monthly basis beginning in 2010. The small work group reviewed the successful components of the program and evaluated ways to implement improvements in the existing pilot oncology nurse navigation program. The following steps were taken:
- A literature review was conducted and resources were identified to aid in program development. The literature review focused on the following topics related to oncology nurse navigation: metrics, program design, core competencies, and clinical roles.
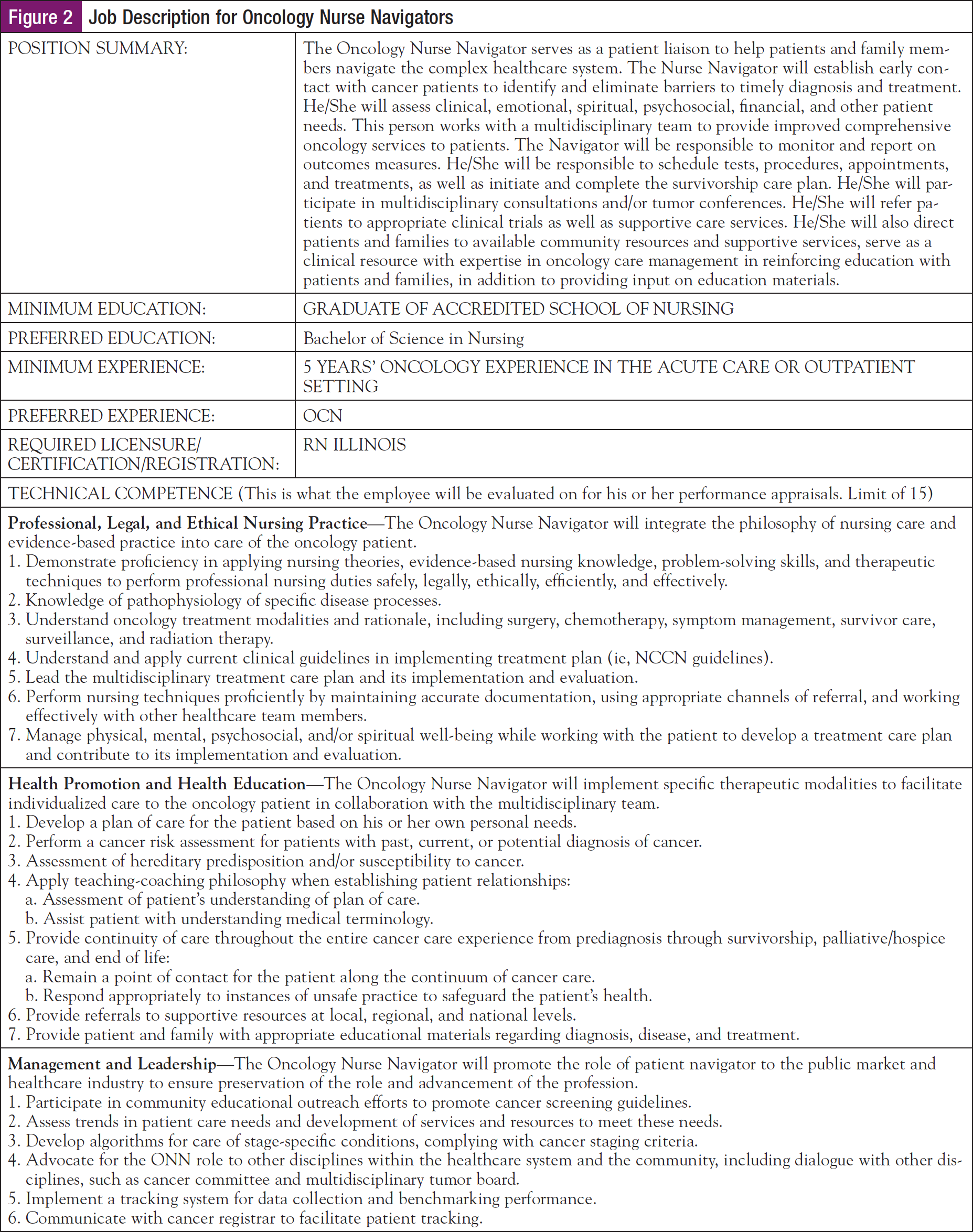
- The job description for the ONN was defined using standardized core competencies. The existing ONN was operating under a general oncology nursing job description that did not include role definitions germane to the ONN role, such as assessment of barriers, actions for guidance through the healthcare system, and patient education competencies. The job description for the ONN was developed using competencies from the National Coalition of Oncology Nurse Navigators (Figure 2).4 The integration of the standardized core competencies into the ONN job description provided structure to the new role and served as a framework for the decidedly diverse role. New hires to the ONN role benefited from the specifics of the job description as the role was clearly outlined as were detailed job expectations.
- The medical director and director of oncology services of the center’s department obtained administrative support at the facility’s executive level from the chief nursing officer and the vice president of patient care. The small work group met for 6 months and then used the information garnered from those meetings to launch an oncology nurse navigation development team.
Multidisciplinary Team Formation
Using information provided by the small work group, the main work team was created and goals were established. The oncology nurse navigation development team sought to achieve quality outcomes in specific areas.
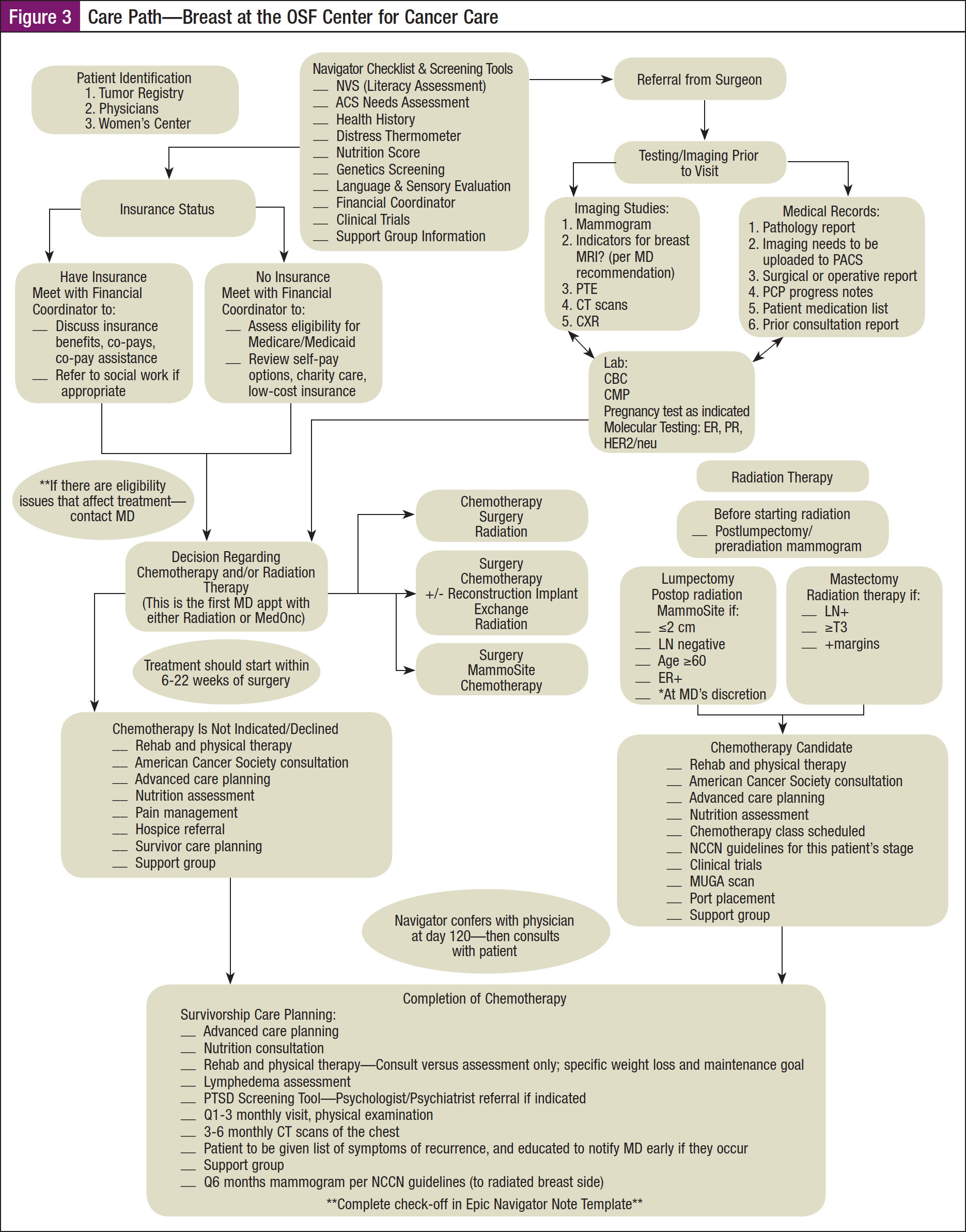
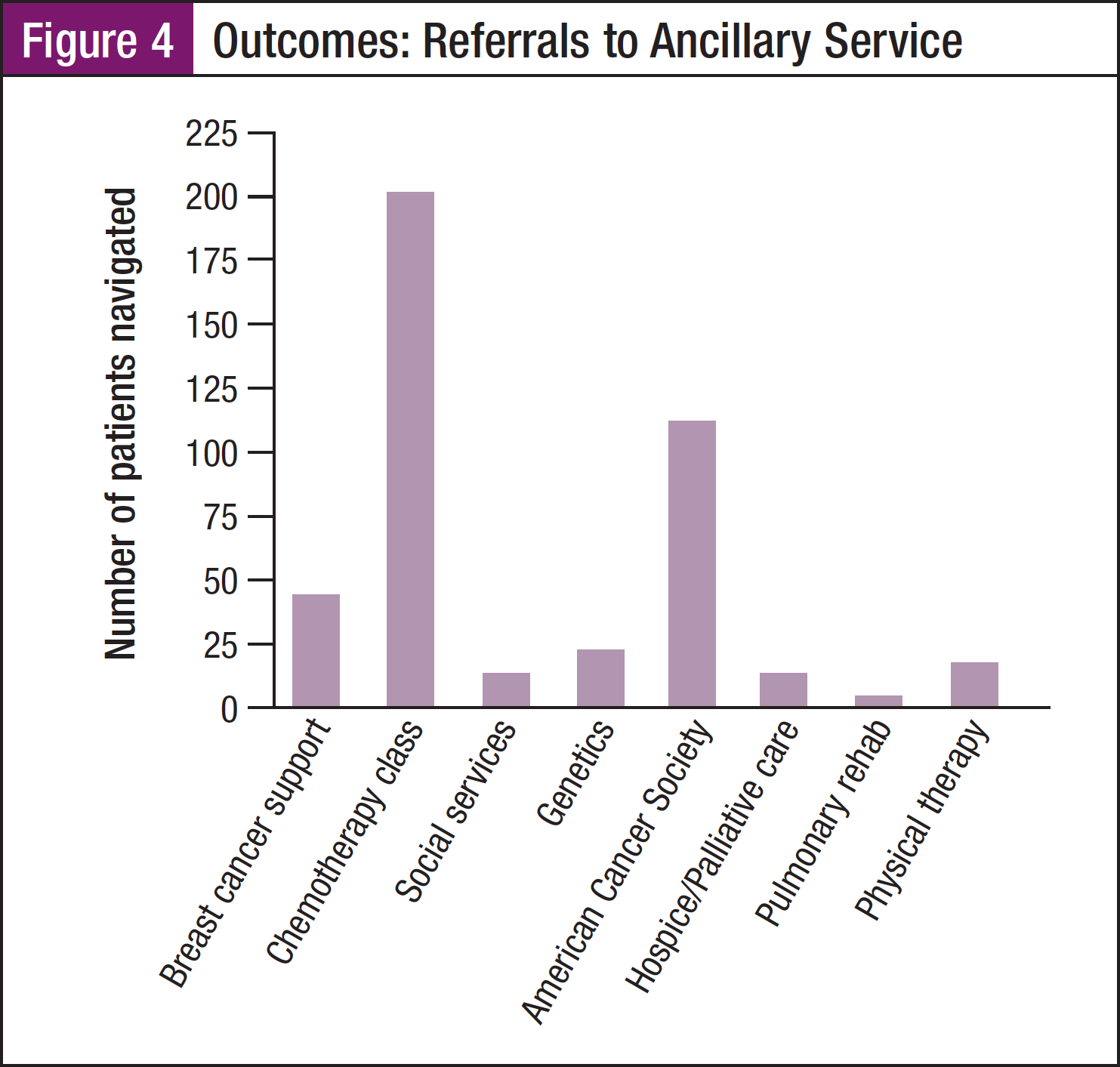
One goal was to increase the number of referrals to ancillary support services, including breast cancer support groups, nutritional services, financial coordination services, cancer rehabilitation, pulmonary rehabilitation, genetic counseling, and chemotherapy education classes. The baseline volume for referrals to ancillary services prior to the initiation of the oncology nurse navigation program was less than optimal with a 60% attendance rate to chemotherapy education classes by all chemotherapy patients. The breast cancer support group referrals were inadequate as well, reaching only 52% of all breast cancer patients. The pulmonary rehabilitation and cancer rehabilitation departments consistently reported low referral numbers each quarter. The team sought to increase the percentages of referrals to ancillary services by 25% in the first 6 months of the program launch.
Given the excellent anecdotal patient satisfaction feedback from the pilot program, a second objective of the new program was to improve patient satisfaction over a wider range of the patients with cancer population. The existing pilot navigation program focused on only 1 disease site, breast cancer, and because the pilot program was a part-time position, the navigator was only able to reach approximately 70% of all breast cancer patients. The intention of the new program was to expand the population of patients under navigation by at least 3 disease sites and to increase the nurse navigation positions from 1 part-time nurse to 2 full-time nurses. It was also the aim of the oncology nurse navigation program to improve efficiency by reducing the wait time from diagnosis to oncology consultation. The standard was set for patients to be seen by an oncologist within 1 week from the time of initial referral to the center. Prior to program initiation, the average wait time from initial referral to oncology consult in all disease sites was 11.9 days.
The team sought to meet the program goals would encompass the accreditation standards put forth by the CoC. The oncology nurse navigation development team consisted of multidisciplinary members including administrative staff, oncologists, oncology nurses, oncology clinical nurse specialists, social workers, pastoral care staff, and community support persons from the American Cancer Society. The team met on a monthly basis and developed methods for assessment and guidance of the program.
Community Health Needs Assessment
In 2013, Saint Anthony Medical Center, along with a collaborative team of health professional experts and key community advocates, conducted a Community Health Needs Assessment (CHNA) in keeping with the federal requirement for tax-exempt hospitals.5 A CHNA is required to be conducted every 3 years and had last been completed by the collaborative team in 2010.
In the interest of meeting the specific needs of oncology patients in the service region and fulfilling the CoC requirements, the data provided by the CHNA were integrated into the guidelines for the oncology nurse navigation program. Specifically, the CHNA report indicated that obesity rates in the service region were higher than the state average, prompting the team to develop a consistent process for initiating cancer rehabilitative referrals within the care map algorithm. The CHNA report showed a regional increase of 11% over the past 3 years in persons reporting that they felt mentally unhealthy on most days. In light of the mental health data, the team developed a system to trigger social service referrals for patients based on the National Comprehensive Cancer Network (NCCN) distress tool score.6
The needs assessment tool provided through the Association of Community Cancer Centers (ACCC)7 was implemented as a means to identify areas that needed to be addressed prior to the initiation of the program.2,3 The tool also assisted the team in considering specific aspects of the navigation program. For example, the ACCC tool aided the team in decision-making regarding which disease sites would be adopted into the navigation program. The top 4 analytical disease sites were chosen: breast, prostate, colon, and lung.
Care Map Development
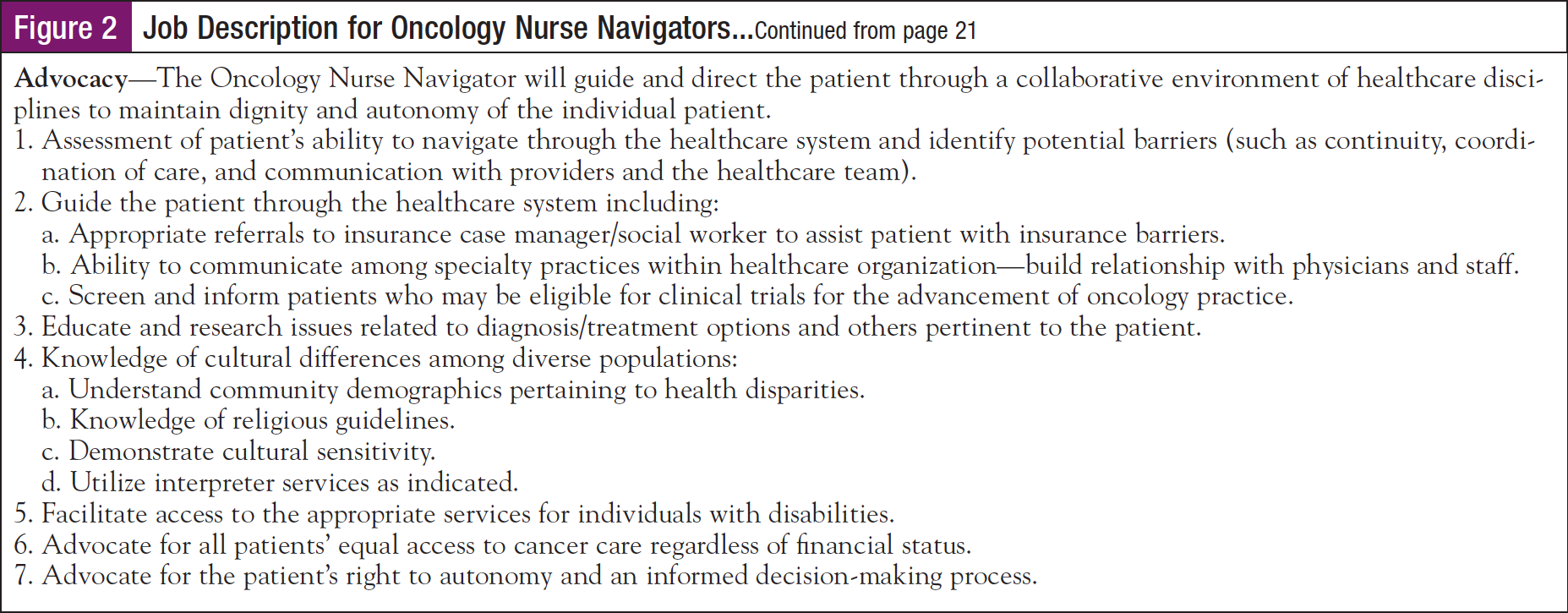
Once the needs assessment was complete, the information obtained was integrated into disease-specific care maps (Figure 3) that were created to serve as algorithms for the ONNs to reference while navigating patients. The information included in the care maps was based upon guidelines from the NCCN and Oncology Nursing Society’s guidelines for oncology patient navigation.7,8
The development of the care maps by the multidisciplinary team has proven to be instrumental in both the improvement and the execution of the ONN program. The care maps guide ONN actions that are vital in terms of meeting national guidelines for best practice, delineating scope of care, ensuring consistency in care delivery, and establishing clear strategies that positively impact outcomes. The care maps expedite diagnostic testing, staging, and treatment for patients, and also assure the integration of education, and supportive, palliative, and survivorship care. Validated screening tools have been incorporated into the care maps, enabling the ONN to properly assess patients and make appropriate referrals to ancillary services based upon the patients’ individual needs.9
Outcomes
For the first 6 months of the advent of the ONN program, all newly diagnosed patients with cancer of the breast, prostate, lung, and colon were navigated—a total of 202 patients. With the increased time and resources devoted to oncology nurse navigation, referrals have been more consistent to support groups, genetic counseling, cancer rehabilitation, pulmonary rehabilitation, hospice, and the American Cancer Society (Figure 3).
The implementation of the ONN program has led to a marked increase in attendance at the chemotherapy class offered in the department as well as increased attendance at the department’s breast cancer support group (Figure 3, Figure 4). In addition to boosting referrals to ancillary services, the oncology nurse navigation program has shown indications of decreasing wait times from diagnosis to oncology consultation. Average time from diagnosis to consult decreased from 11.9 days (for all new patient referrals to the prenavigation program) to 5.5 days (for patients in the navigation program).
Survivorship Care Planning
The care maps include guidance for survivorship care planning recommended by NCCN6 and the survivorship section of the care maps have been integral in the development of the survivorship care planning process.
Currently, the survivorship care planning process includes a computer-based template that is populated with patient-specific information containing treatment dates and doses. The survivorship care plan information is finalized by the ONN and presented to the patient on the first follow-up visit with the oncologist after treatments are completed. The survivorship care plan is printed and included in a survivorship folder complete with information about the challenges of survivorship and resources for specific supportive programs. The survivorship care plan is faxed or mailed to the patient’s primary care physician once treatment and the survivorship visit have been completed.
Next Steps
The ONN program has proven to be a valuable service that positively promotes referrals to ancillary and community support services. The next steps for ongoing program improvement include the following:
- Development of additional care maps for disease sites that will be added to the ONN program in the future—including cancers of the head and neck and pancreatic cancer.
- Streamlining the survivorship care planning tool and process to ensure all patients who have received navigator services are provided with a survivorship care plan upon treatment completion.
- Implementation of a patient satisfaction survey for the oncology nurse navigation program.
Author Disclosure Statement: All authors have nothing to disclose.
Corresponding Author: Peggy Malone, RN, BS, OCN, OSF Saint Anthony Center for Cancer Care, 5666 East State Street, Rockford, IL 61008. E-mail: Peggy.e.malone@osf healthcare.org
References
- Commission on Cancer. Cancer Program Standards 2012: Ensuring Patient- Centered Care. Version 1.2. http://www.facs.org/cancer/coc/programstandards 2012.pdf. Accessed July 24, 2014.
- Campbell C, Craig J, Eggert J, Bailey-Dorton C. Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncol Nurs Forum. 2010;37:61-68.
- Christensen D, Bellomo C. Using a nurse navigation pathway in the timely care of oncology patients. J Oncol Nav & Survivorship. 2014;5:13-18.
- National Coalition of Oncology Nurse Navigators. www.nconn.org. Accessed August 6, 2014. http://www.irs.gov/Charities-&-Non-Profits/Charitable-Organizations/New- Requirements-for-501(c)(3)-Hospitals-Under-the-Affordable-Care-Act. Accessed August 26, 2014.
- National Comprehensive Cancer Network. www.nccn.com. Accessed July 28, 2014.
- Association of Community Cancer Centers. www.accc-cancerorg/resources/ pdf/PNTOOLS/Pre-Assessment-Tool.pdf. Accessed July 24, 2014.
- Oncology Nursing Society. Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers Joint Position on the Role of Oncology Nursing and Oncology Social Work in Patient Navigation. https://www.ons.org/about-ons/ons-position-statements/education-certification-and-role-delineation/oncology-nursing-0. Accessed July 28, 2014.
- Swanson J, Koch L. The role of the oncology nurse navigator in distress management of adult inpatients with cancer: a retrospective study. Oncol Nurs Forum. 2010;37:69-76.